Coronary artery disease
The heart is essentially a muscle. The only muscle in the body that works 24 hours a day!
To be able to take care of such a heavy workload, it needs a continuous supply of blood.
The tubes that carry oxygen rich blood are called arteries. Arteries of the heart are called 'Coronaries'.
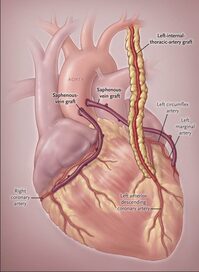
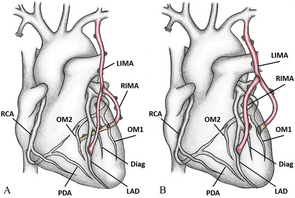
There's one left main coronary artery (LM) and one right coronary artery (RCA).
The left main coronary divides into two branches - LAD and Circumflex (Cx).
If blocks develop in any or all of these coronaries, then the heart muscle beyond the block is deprived of blood and this can result in symptoms like chest pain or tightness (angina), breathlessness (dyspnea), fatigue, palpitations, dizziness, blackout.
Typical pain is on the left side of the chest and goes down the left arm, But, it may at times be in the back, jaw, shoulder. More often than not, pain is following exertion.
Sometimes pain may not be felt. Especially, in diabetics. Or those having good collaterals (additional blood flow pathways)
If the chest pain is severe, not getting relieved with rest, associated with sweating, nausea and vomiting, it may indicate an oncoming heart attack and immediate admission to a hospital is advisable. Preferably, one with facilities and expertise for immediate coronary angioplasty (called PAMI).
If it turns out that heart evaluation is normal, it's ok. Better safe than sorry!
Risk factors for developing these blocks (called atherosclerotic plaques):
Diabetes, High blood pressure (Hypertension), Bad cholesterol and other lipid (fat in the blood) levels, history of heart attack/sudden death in close biologic family members, stress, smoking.
If your doctor tells you that it's a heart attack, then it can be of two types:
STEMI - abnormal changes in ECG or
NSTEMI - normal ECG but raised Troponin (chemical released in blood due to injury to heart muscle).
You may be either be advised immediate coronary angioplasty (called PAMI) or clot dissolving therapy (Thrombolytics) depending on time since onset of severe chest pain. Immediate dissolving of the clot will prevent the heart muscle from permanently damaged. Thus time is of utmost importance. TIME IS MUSCLE !
A heart attack is usually treated in the hospital with pain control, oxygen, blood thinners and NTG drip (will improve blood flow in coronaries).
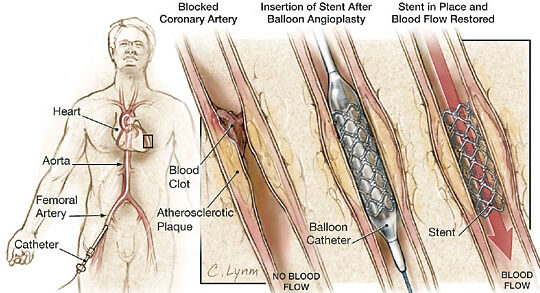
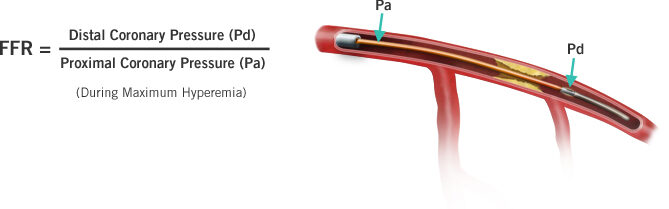
A coronary angiogram is done to know the presence and types of blocks in the coronaries. It may be done through the groin or the wrist. It's currently the gold standard for understanding the coronary road map. At times, a special investigation called FFR may be done to guide the cardiologist in selecting the best treatment option for you.
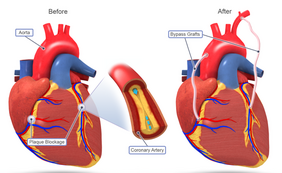
If severe blocks are noted in all three coronaries, then either surgery (bypass called CABG) or angioplasty (PCI) will be advised depending on various factors - diabetes, site of blocks, length of block, amount of calcium in blocks, etc.
Thrombolysis is done by cardiologists or MD (General Medicine) physicians.
Angioplasty (PCI - primary coronary intervention) is done by interventional cardiologists.
Surgery (CABG - coronary artery bypass grafting) is done by cardiac surgeons.
In Thrombolysis, the block in the coronary artery is broken up in order to restore blood flow.
In PCI, a guidewire with a collapsed balloon on it is inserted via the groin/wrist into the coronary artery and positioned across the block. The balloon is then opened up, stretched and block broken down. A drug releasing stent (wire meshwork) is then inserted at that site.
In CABG, tubes are taken from the inside the left chest wall (LIMA - left internal mammary artery) and the arm (radial artery) / leg (veins). These are used to go around the block in the coronary artery. Thus called 'bypass'. Almost always, LIMA is attached (grafted) to thy most important artery of the heart (LAD).
Both CABG and PCI are safe procedures in straightforward cases with risk to life less than 1%.
Risk in some case may vary depending on LVEF, associated illness, age, recent heart attack, target vessel beyond the blocks, need for additional surgery, first or redo surgery, etc.
The condition of the main pump of the heart, left ventricle (LV) is important in knowing the risk involved.
It is known as LVEF (left ventricular ejection fraction) -
Normal - 60% or more.
Mildly decreased - 40 - 60%.
Moderately decreased - 30 - 40%.
Severely decreased - less than 30%.
Inquire from your treating doctor about risks involved, alternative options, risk-benefit ratio and make a decision about proceeding with the proposed procedure.
Common risks at CABG - infection, bleeding, stroke (brain injury), kidney failure, need for IABP and risk to life. All of these are usually 1-3%. Can, at times, be more if there are complicating conditions before surgery. Your doctor will tell you about these.
If you are on blood thinners, these need to be stopped 3-5 days before surgery. Unless it's an emergency.
IABP - balloon pump inserted over a wire through the groin to aid the heart in critical conditions before surgery.
Very rarely, a permanent pacemaker may be needed after surgery for some types of blocks in the electrical circuit of the heart.
By and large, both CABG and PCI are commonly done procedures with excellent results translating into improved survival and quality of life.
All open heart surgeries need availability of four units of blood. They may not all be used but have to be on standby. Ensure that friends are relatives are available as donors. Sometimes, blood products (FFP, Platelets, Cryoprecipitate) may also be needed.
Most patients (~95%) are discharged 5-7 days after straightforward surgery. In complex cases, the stay may be more.
After discharge from the hospital, it is important to do breathing exercises taught to you. Typically, it will also involve breathing in and out of a small machine (spirometer) 10 times every hour that you're awake. This is usually for 2 weeks from discharge.
A chest belt (corset) needs to be correctly worn for 3 months after surgery. It should not be so tight that you have pain or difficulty in breathing. But, tight enough that it serves the important function it's meant to do.
A gradual increase in your walking is to be done after surgery. Start at 100 metres for two days, then 200 metres for two days and so forth, Typically two weeks after surgery most patients can walk upto a km at a time (around 15 - 30 minutes).
Do not lift weight more than 5 pounds for three months after surgery.
Consult the dietician in the hospital for advice on diet after you go home - low cholesterol, low saturated fat.
CABG
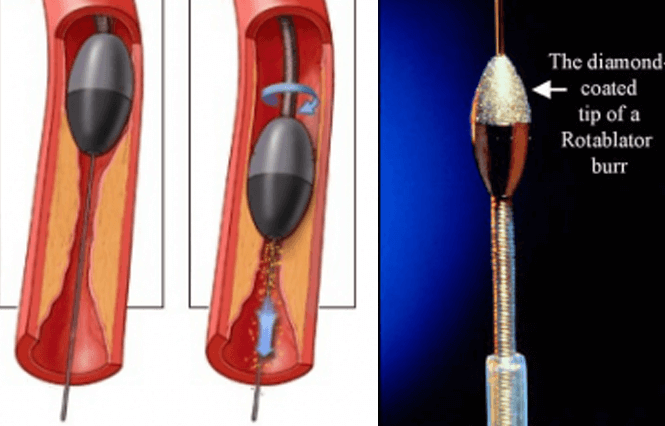
PCI FFR Rotablation